
Science in Christian
Perspective
on Ethics
The Future of Medical Science:
Ethical and Theological Implications, Part II
Jay L. Hollman, M.D.
Ochsner Clinic of Baton Rouge
16777 Medical Center Drive
Baton Rouge, LA 70816
From Perspectives on Science and Christian Faith 47 (March
1995): 23-31.
© 1995 Americian Scientific Affiliation
Ethical issues in medical science in the 1990s will be numerous, occur in all disciplines of medicine, and affect all physicians. To discuss future medical ethical issues in a relatively short space, it is tempting to choose one of two extremes. One extreme is to simply catalog all ethical problems arising from new discoveries or emerging technologies, while the other extreme would be to choose one ethical issue as most important and attempt to cover it in depth. In this two-part paper, I have chosen a middle ground, providing some background on five issues in medium depth: (1) euthanasia, (2) fetal tissue transplant, (3) psychiatry and neuroscience (specifically the issues raised by homosexuality), (4) health care costs and the ethics of cost containment, and finally (5) preventive medicine, particularly as it relates to sexually transmitted diseases including AIDS. I hope to supply some background information on these selected issues and to stimulate further reading and research.
Future Issues in Psychiatry and Neuroscience
How one views homosexuality scientifically affects the way one regards the morality of this condition. If homosexuality is due to a genetic defect or a deficiency of certain brain cells in a particular area of the hypothalamus, then discriminating against homosexuals could be likened to discrimination by race or gender.
One of the primary goals of militant groups, such as the AIDS Coalition To Unleash Power (ACT UP), is to eradicate the social ills of racism, sexism, and homophobia (Wachter 1992). These groups will use science to support their argument. The genetic work of Bailey and Pillard (Bailey 1991) and the neuropathologic work of Simon LeVay (LeVay 1991) have given empiric evidence to the concept that homosexuality is decided by nature and not by nurture.
The study of Bailey and Pillard studied monozygotic twins, dizygotic twins, and adoptive brothers. This study confirmed earlier studies that showed a concordance in sexual orientation for monozygotic or identical twins compared to dizygotic or fraternal twins. An identical twin to a homosexual had a 50% chance of being homosexual. A fraternal twin was no more likely to be homosexual than an adopted brother to a homosexual. These twin studies imply a genetic component to homosexuality but do not take it to necessity. An absolute genetic trait such as eye color would show 100% concordance.
The search for a difference in the homosexual's brain structure has
centered in the hypothalamus because of nonhuman primate studies suggesting that the
regulation of male sexual behavior be found in the hippocampus. The study of LeVay
measured the volumes of the interstitial nuclei of the anterior hypothalamus (INAH) in
women, homosexual males, and heterosexual males. Differences were found in INAH 3. The
homosexual males had a reduction in cells in this nucleus similar to normal females. The
conclusion from this study might be that homosexuals are homosexuals because of structural
differences in their brain. Thus, unlike Romans 1 implies, they do have an excuse.
nonhuman primate studies suggesting that the
regulation of male sexual behavior be found in the hippocampus. The study of LeVay
measured the volumes of the interstitial nuclei of the anterior hypothalamus (INAH) in
women, homosexual males, and heterosexual males. Differences were found in INAH 3. The
homosexual males had a reduction in cells in this nucleus similar to normal females. The
conclusion from this study might be that homosexuals are homosexuals because of structural
differences in their brain. Thus, unlike Romans 1 implies, they do have an excuse.
This study has several deficiencies: First, the homosexual population died primarily of AIDS. Equally important is the fact that there is a great deal of overlap; some heterosexuals had a small INAH 3, the same size as homosexual males. If these structural defects are real, one might expect hormonal differences between heterosexual males and homosexual males but in fact these have been looked for extensively and there are none (Hendricks 1989). Furthermore, if homosexual behavior was determined by structural changes in the brain then one would expect homosexual behavior to be present in all cultures. In fact, homosexual behavior is absent in many cultures. Moreover, homosexuals have been shown to completely change their sexual orientation. Eleven homosexuals studied by Pattison showed an abrupt and radical shift in their sexual orientation following their conversion to Christianity. At an average of four years following conversion, all eleven were functioning as heterosexuals. Three patients still had some evidence of neurotic conflict, but eight were emotionally detached from homosexual identity in both behavior and intrapsychic process (Pattison 1980). This study suggests that homosexual orientation could be a spiritual disease and not due to structural changes in the hypothalamus.
Homosexuality has been associated with greater depression and general unhappiness. Militant homosexual groups might argue that this difference is due to societal ostracism. Equally possible is the hypothesis that homosexuality is an abnormal lifestyle and, because of this, homosexuals are unhappy and depressed. Freudian psychiatrists argue that homosexuality is due to an abnormal family dynamic with a mother's contempt for an overly passive or an overly aggressive father and the son's refusal to accept the male role. The Freudian psychiatrist forms an uneasy alliance with the evangelical Christian in calling homosexuality a problem.
Despite how this recent data is interpreted, Bailey clearly believes homosexuality is decided by prenatal brain development. This hypothesis challenges the Christian concept of homosexuality as sin. No absolute genetic or structural connection has yet been identified. Even identifying a predisposing hypothalamic lesion or proving a 50% concordance among monozygotic twins does not excuse sin any more than the demonstration of a genetic predisposition toward alcoholism excuses the individual alcoholic. This argues only for original sin; man has a genetic predisposition to sin. If science can discover to which sin a person is predisposed, it might be helpful to that person. For example, a child of two alcoholics would be advised to avoid mood altering drugs and a brother of a homosexual should avoid behavior predisposing to homosexuality. Males with an extra Y chromosome (XYY) are twice as likely to go to prison; thus, they should be schooled in gentleness and respect for authority.
A genetic predisposition does not excuse sin because we all have our own peculiar weaknesses. We all sin; our expressions are only different. Scriptural teaching on homosexual practice is clear (see Lev. 20:13 and Romans 1:26,27). If the practice of homosexuality is sin, then the solution must come from the transforming power of the Holy Spirit acting through the Christian life. This is precisely what Pattison described. After conversion to Christ, homosexuals in his study became involved in support groups and small group Bible studies. Accepting homosexuality as sin and trusting Christ to transform their sinful nature was the first step toward changing to normal heterosexual relations. Charles Colson in his book, The Body, describes several groups working in the church that are helping homosexuals convert to heterosexuals (Colson 1992). This is the Christian solution to the problem of sin in general and to this sin in particular.
Understanding certain chemical imbalances in the brain and showing them through positron emission tomography or other brain mapping techniques will accentuate the conflict between structural or functional changes in the brain and human responsibility. If abnormal neurohumoral transmission can be identified in a depressed patient, does this explain his depression? Is this person no longer responsible for certain behaviors associated with his depression? The answer from theology is that man is both sinful and accountable. The ability to discover defects that predispose one to sin or occur because of sin does not excuse man.
The 1990's have been designated as the decade of the brain because of the anticipated great number of discoveries that will result from new modalities of investigation; we will learn that neurological defects and neurotransmitters are associated with certain behaviors. But structural and functional defects do not excuse man; they merely delineate and describe individual manifestations of the sin nature.
Health Care Costs
Medical and governmental groups have conducted studies on health care costs. Whether such studies can be considered science or not is open to debate. Nonetheless, there are many ethical issues involved in the current health care financial crisis. As a background, it is important to understand the source of increasing health care costs. It is not all due to high technology. Within this background, two ethical issues should be exposed: first, the injustices in the current health care system and second, ethical problems with proposed solutions to the health care crisis that involve false alternatives.
The cost of the current health care system and its rate of growth are a great concern for government and industry in the United States. The United States may spend 14% of its gross national product on health care this year. This exceeds by several percentage points the amount spent in other industrialized nations for health care. In the global economy, it means that our products for export will be more expensive because of health care costs. An analysis of the way the money is spent is particularly troublesome. While 19% of total U.S. health dollars are spent on physician fees, 20-24% of health care dollars are spent on administration (Weissman 1992).
Since 1970, the number of health managers and administrators in the United States has grown at four times the physician rate. The U.S. spends $497 for health care management compared to $156 per capita in Canada (Weissman 1992). The United States with 5% of the world's population has 70% of the world's attorneys. Their litigation and threat of litigation have added billions to the cost of health care, new device development, and new drug development. Dow Chemical spends 40 cents on every dollar received from silicone breast implants on legal and regulatory fees (Fisher 1992). Ethically this creates problems for physicians who wish to lower health care costs. In Louisiana, an obstetrician will spend nearly $30,000 per year on medical malpractice, a neurosurgeon over $46,000 (see Table 1). Louisiana has a cap on malpractice suits so that these figures are relatively low. In some areas of the U.S., such as southern Florida, similar malpractice coverage is over $100,000 per year.
If medicine becomes more expensive, it will put Americans out of work. If one attempts to lower costs without compromising care, serious efforts to reduce administrative and legal costs must be pursued.
There are many injustices in the current medical system. So-called cost shifting has made the amount of money received by a hospital for a given procedure vary 2-3 fold. For example, the standard cash price for an angioplasty might be $22,000. Medicare might pay $8,800, Medicaid might pay $3,000, and an insurer with a special contract might pay $9,500. In order for hospitals to break even, they raise the cash price to such a ridiculous amount that the poor, uninsured, or underinsured are strapped with a lifelong debt to the hospital.
The current system of reimbursement favors procedures over cognitive skills. This system has resulted in a predominance of specialists over primary care doctors. The number of specialists in Canada and most European countries is limited. In Canada one-half of the physicians are primary care physicians, while only one-third of U.S. physicians are primary care physicians (Whitcomb 1992). More specialists result in more procedures per capita whether the procedure is a hysterectomy or a coronary bypass. Physicians choose the specialty based partly on projected future earnings and their own indebtedness following medical school. While many specialists improve access to specialty care, there is a greater potential for abuse since more marginally-indicated procedures may be performed.
Our current system of competitive medical units does not often consider the needs of the community or country when making decisions. Training programs for specialists are often large despite the lack of need for these specialists because the institution wants to use resident physicians to help with patient care. Although a town might have little need for another Magnetic Resonance Imaging (MRI) scanner, an individual hospital might acquire such a scanner for its own financial benefit. This policy has lead to a proliferation of technology. Americans enjoy the convenience of good access but at the cost of efficiency. At present no one has the economic motivation or the legal power to assist the community or the country as a whole to limit the application of new technology. This adds to overall medical costs.
Finally, proposed solutions to the health care crisis create further ethical dilemmas. The Oregon paradigm of prioritizing health care by disorders and not funding Medicaid payment for low priority items has been widely watched as a potential solution to rising health care costs. The proposal has some merit in that it eliminates public funds for truly dubious procedures such as sex-change operations and aggressive treatment of end stage AIDS. It also tries to look hard at cost effectiveness. By initially denying experimental solid organ transplant payment, it has caused us to realize that the dramatic new therapy is not always cost effective. The cost per year of life saved is over $40,000 per year for a liver transplant and $28,000 for a cardiac transplant. Since the cost was great and the numbers benefited small, Oregon initially chose not to fund such treatment. By not funding some solid organ transplants and not funding the treatment of intervertebral disc disease, chronic pancreatitis, and other disorders for which there exists effective therapy, Oregon is saying that there is not enough money to treat everyone, especially when the cost benefit ratio is relatively low.
Before one can ethically deny beneficial health care to an individual
based on cost alone, one must be very sure that the health care house is in order. As
outlined above, there is a great need for improvement. Reducing legal fees, administrative
costs, and redundant medical services should be done prior to eliminating public funds for
the potentially beneficial therapies. We, as a society, must choose between a $2 million
legal award to the family of a deceased victim of dubious malpractice or the funding of
back surgery for 40 living patients with herniated discs.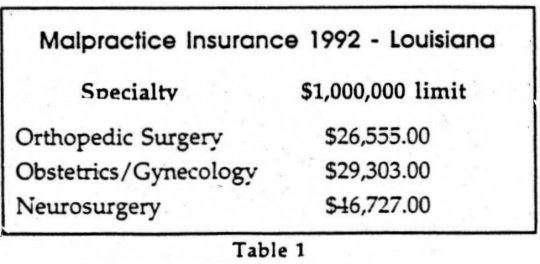 Which shall we choose? Shall we
have medical redundancy with complete service hospitals convenient to every corner of the
community or shall we centralize high tech services to allow full utilization so that we
can continue to offer truly beneficial procedures to the indigent?
Which shall we choose? Shall we
have medical redundancy with complete service hospitals convenient to every corner of the
community or shall we centralize high tech services to allow full utilization so that we
can continue to offer truly beneficial procedures to the indigent?
It is well beyond the scope of this paper to propose a comprehensive solution to the health care crisis but there are some ethical issues at the crux of the solution. A major reason for the increase in administrative costs is a lack of trust. Physicians do not trust insurance carriers and insurance carriers do not trust physicians. According to the Wall Street Journal, this lack of trust has created a $7 billion medical review industry. Insurance companies employ armies of nurse reviewers for concomitant review of patient care. This nurse will call the physician's office every 1-2 days checking on the patient's progress, encouraging early discharge. The Professional Review Organization (PRO) is charged with the review of Medicare patients. This group employs nurses and physicians to review the charts of Medicare patients after their discharge to assure the federal government that quality of care standards are being met. If the medical record is inadequate to justify the diagnosis or the treatment employed, the Medicare payment for service will be denied. Physicians who achieve negative points from PRO reviewers will be subjected to comprehensive reviews. If enough negative points are accumulated, they will lose payment under the Medicare system.
In 1990, the inspector general looked at the effectiveness of the review organization with respect to cataract surgery; the conclusion was that the U.S. paid $13.3 million to utilization reviewers to save $1.3 million in possibly unnecessary cataract surgery (Burton 1992). Hospitals, to defend themselves from a loss of payment from PRO reviewers, employ their own nurse reviewers to assure that the patient's chart is in proper order before patient discharge. Other nurse reviewers monitor Medicare and HMO patients' length of stay to maximize reimbursement and avoid loss of payment. The University of Chicago had 15 employees and paid a total of $1.2 million per year to answer utilization review (Burton 1992). Hospitals employ consultants to educate physicians on proper charting to avoid loss of Medicare payment and to list any possible diagnosis to maximize Medicare payment. Paying people to copy thick charts for review adds further to the administrative cost of health care.
If there is a lack of trust among physicians, hospitals, and insurance carriers, there is a good reason for this. It is estimated by U.S. News and World Report that fraud could account for nearly 10% of the $817 billion spent on health care this year (Witkin 1992). Physicians have begun advertising, often unprofessionally. Many physicians have become quite wealthy. Physicians have been poor at policing their own ranks. Hospitals have changed greatly from the early church affiliated hospital that saw its work as a mission to today's for-profit hospital that seeks to maximize return and views other hospitals as competition. This mentality has become the guiding force in not-for-profit hospitals also. Chief executive officers of the for-profit hospital chain may make over one million dollars per year in salary and stock options. These large salaries make physicians skeptical that the hospital administration acts in the best interest of the community or in the best interest of the patients. Thus, any solution to the health care financial crisis must address the lack of trust among insurers, physicians, and hospitals. This lack of trust in part reflects a system that had not been responsive to direct market forces. Lack of integrity and greed on an individual and corporate level has created much of the rise in medical health cost. The legal industry in this country has been very successful at capitalizing on this lack of trust.
For the past 10 years, I have been involved with a reuse program for coronary angioplasty catheters. This concept has been borrowed from the developing world where reuse is essential. Minntech, a Minnesota company, has developed a system that systematically cleans and sterilizes coronary angioplasty catheters. These plastic catheters, specifically labeled "for single use only" by the manufacturer, cost over $600 each. By selective reuse, hospitals could greatly reduce their budget for disposables that now consumes 10-15% of their budget. Reuse would also reduce the amount of biohazardous garbage produced by the country. The barrier to reuse is not scientific; the emotional fear of AIDS transmission is unfounded as the AIDS virus is easily killed. The barrier is in part the manufacturer's resistance, in part the Food and Drug Administration's regulation, and in part the fear of legal suits. Even groundless legal suits take years to defend and cost millions in legal fees.
Any solution to the health care crisis that limits care but does nothing to reform the current system is ethically unsound. It creates a false alternative: the only method to reduce care cost is to ration care. It is better to ration greed and litigation and to increase individual and corporate integrity.
Preventive Medicine
Acquired Immune Deficiency Syndrome (AIDS) will move increasingly to
center stage as the prevalence of the disease increases and the disease spreads to the
heterosexual population. In 1992, there were more productive years lost due to AIDS than
to heart disease although heart disease killed over 12 times as many (see Table 2).
Because AIDS kills a younger age on average, the impact on productive years is greater.
Only cancer causes a greater loss of productive years. If projections continue, AIDS will
soon overtake cancer. Thus, for the 1990's, the prevention of AIDS should be the most
important preventive medicine priority.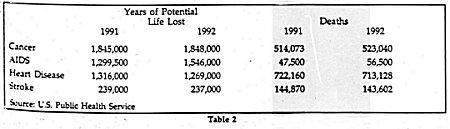
There are many Christians who are calloused to AIDS victims and believe that AIDS is God's judgment on homosexuality, intravenous drug use, and promiscuity. Yet this fairly simplistic explanation fails to account for the one million babies in sub-Sahara Africa who acquire AIDS in utero from their mothers or for the innocent faithful sex partners who acquire AIDS from their promiscuous spouses. This is especially true in Africa where AIDS is spread through heterosexual sex; usually the wife is faithful and receives the virus from her husband. Male to female transmission occurs more easily.
One need only see one young child under five suffering from AIDS to change from indifference to compassion. After seeing such children, you, like I, will earnestly seek a scientific cure for AIDS. Yet, because of the intracellular location of the virus and the unique characteristics of the retrovirus infection, a major curative breakthrough is not expected in the foreseeable future. Immunization effective in preventing viral infections, such as polio and measles, is not effective in preventing AIDS. The presence of antibodies to rubella in the would-be pregnant female assures the potential mother and her fetus of protection from measles caused by rubella virus. Antibodies to the AIDS virus are produced by every person infected by AIDS. However, they do not prevent the development of the disease because the AIDS virus directly attacks the immune system.
If curative medicine and usual preventive medicine through vaccination offer no reasonable hope for prevention of the AIDS epidemic, what does? Barrier methods, especially the use of the condom, have been advocated as has extramarital sexual abstinence. From a scientific and public health perspective, each method requires different societal support and promises different outcomes.
The use of the condom for AIDS prevention sanctions continued promiscuity. Making condoms freely available through the school health nurse has the effect of condoning extramarital intercourse. Since the public health service advocates the use of condoms, it provides the blessing of authority and a false sense of security. Users feel that condoms can always prevent AIDS. In fact, condoms can become dislodged during intercourse; they are associated with a definite pregnancy risk despite conscientious use. The AIDS virus is much smaller than human sperm.
Condoms, if used properly, will reduce the probability of infection
with the AIDS virus but will not provide absolute protection. This is one reason why the
use of the female condom has been advocated and will soon be marketed in the U.S. and
Europe. Clinical trials in massage parlors in Thailand have shown that while the male
condom provides 50-60% protection from sexually transmitted disease in coital acts, an
additional 15-20% can be protected using the female condom (Global
AIDS News). The application of this complex methodology with scrupulous attention to
detail is problematic in the predictable passion of romantic love as practiced in this
country among teenagers. A Center for Disease Control survey of sexually active high
school students revealed that only 46% reported that they or their partner used a condom
at their last sexual encounter (Morbidity and Mortality Weekly
Report 1992). Advocating barrier methods is offering a less effective method of
protection from AIDS compared to abstinence.
compared to abstinence.
Furthermore, barrier methods are economically impractical in the developing world where AIDS prevalence is highest. A 50-cent condom could represent 50% of a man's daily wages in East Africa. In the country of Uganda with 18 million inhabitants, an estimated 600,000 sexual acts are performed daily. To supply barrier protection for all citizens would require more than the total Ministry of Health's budget.
If abstinence and marital monogamy are the best form of protection against AIDS, what prevents the widespread application of this technique? This ethical issue in public health and preventive medicine has personal and existential ethical implications. According to USA Today, 60% of females and 73% of males at 19 years old are sexually active outside of marriage. About 25% have sex regularly, 50% have had two or more sex partners.
The majority of adults in the U.S. are guilty of extramarital intercourse. To suddenly prescribe absolute moral chastity, is to tinker with societal permissiveness and individual freedoms - two values deeply cherished by the majority of Americans and especially the intellectual elite. Historians have traced these values to science. Science and scientists have always had influence outside the direct impact of their discoveries.
Historian Paul Johnson has stated in his book Modern Times that the impact of Einstein and Freud have been uniquely used as intellectual priests in moral relativism. Because of the widespread circulation of the theory of relativity in the 1920's, the absolutes of Newtonian physics had been dethroned. Absolute time and absolute length were no longer and all motion was curvilinear.
At the beginning of the 1920's the belief began to circulate, for the first time at the popular level, that there were no longer any absolutes: of time and space, of good and evil, of knowledge and above all of value. Mistakenly but perhaps inevitably, relativity became confused with relativism. (Johnson 1983)
This lack of absolutes greatly distressed Einstein so he devoted the later portion of his intellectual life trying to anchor his physics to field theory; he greatly disliked uncertain principle, stating in a letter that he believed in law and order but not in a God who plays dice with the universe.
Freud, the other scientific high priest of modern relativism, was antireligion in his philosophy. For Freud personal guilt feelings were an illusion to be dispelled (Johnson 1983). Freud's effect on society has gone far beyond his scientific contribution. Freud's gospel was an agnostic cult - there is a secret and special sexual meaning to people's motives and actions. Sexual overtones could be seen in all of life's activity. The oral phase, the anal phase, the Oedipus complex and the Freudian slip were all means of understanding life in sexual terms. Free sexual expression was the logical consequence of freedom from the harsh super ego. Sexual innuendo and sexual joking have dominated sexual discussions from bars to operating rooms until slowed by legal threats of sexual harassment. It has been popular to believe that we should be obsessed with sex. This was a natural corollary to Freudian teaching.
With the license of birth-control pills in the 1960's and the backup system of abortion on demand in the 1970's, promiscuity has been on the rise. Believers in evolution and the survival of the fittest could take existential satisfaction in having multiple sexual partners or conquests. The introduction of AIDS into the paradigm and especially the unequivocal scientific evidence that abstinence is the superior method of prevention should cause much questioning of the moral relativism of the 20th century. Here is an absolute and if this absolute exists then there may be others. Condoms are embraced as a means to avoid an encounter with an absolute.
For the individual, there is the realization that guilt also may be real. There is no means in the modern Freudian paradigm to deal with real guilt. While few commit the sin of actual murder and the sin of lying is easily dismissed, there is something so concrete about sexual sin that it cannot be dismissed. If 70% of adult men are guilty of this sin, then lifting high the standard of abstinence might have a tremendous psychic cost unless the forgiveness through Christ's atonement can also be offered. The ethical dilemma of preventive medical science is the final stop to the ultimate ethical dilemma for the individual: to deal with moral absolutes and his personal sin.
If we are to create a society where marital monogamy is the standard, there will need to be major changes that differ from classic preventive measures. If closing of the gay bathhouses and notification of sexual partners were viewed as a violation of privacy by the gay community, imagine the public outcry that might come from efforts to ban pornographic literature and to censor from commercial television programs that exalt promiscuity. All these are logical decisions if we are to move toward a society where moral faithfulness will be the standard. The scientific data (Minnery 1986) gathered from controlled exposure of college males to pornography and public confessions of rapists and other perpetrators of violent sexual crime clearly demonstrate the corrupting influence of sexually explicit materials. Thanks largely to child pornography, more boys and girls are infected annually with sexually transmitted disease than were stricken with polio during the entire 1942-53 epidemic (Minnery 1986). We are only now clearly seeing how later medical illnesses are often linked to childhood sexual abuse. Not only do adults, sexually abused as children, suffer from more frequent psychological difficulties such as anxiety and depression, impaired interpersonal relationships, and suicidal behavior, they also have a higher incidence of chronic pelvic pain, gastrointestinal distress, premenstrual difficulties, and somatic complaints and sleeping difficulties. Sexually abused women are more likely to use cigarettes, have a greater number of sexual partners, and avoid regular preventive care measures (Briere 1992). Thus, the impact of sexual abuse facilitated by pornography has health implications for the next generation as well as for this generation.
If it were possible to prevent or decrease sexual permissiveness in our society by banning pornography and changing the media, then we might improve the health of the next generation on many fronts. Our public prevention programs must present measures to prevent sexual impurity. But sexual purity does not come just from censoring the media and closing public areas that encourage the spread of disease (such as gay bathhouses) but from changing the heart of man from within by the power of God. It is cruel to prohibit teenagers from doing an act and not help them change from within. Moreover if we are to teach that there are moral absolutes and therefore real guilt, we must be kind and offer the forgiveness of God through the atonement of Jesus Christ. Therefore, kindness requires that the gospel and AIDS prevention be linked.
Although I have tried to draw the above argument as cogently as possible, it does not mean that secular man will accept this. Because he starts with different presuppositions, he will interpret the scientific data regarding AIDS differently. Formulating a viable public health policy in a pluralistic society is much different from constructing policy where the Christian world view is accepted. Open, honest, nonviolent, and respectful dialogue between Christian and secular scientists offers the best opportunity to influence public policy. Tact, diplomacy, and even compromise will be a part of these discussions. The resultant public health policy will likely not be completely true to pure Christian ethics but it will be better than policy formulated in the absence of Christian scientific input.
Conclusions
These medical ethical issues challenge us to move from Biblical truth to social action. We must make our culture aware of the weakness of the scientific evidence supporting the hypothesis that homosexuality is due to innate constitutional differences; we must lovingly tell them that this is sin. More importantly the church must demonstrate the transforming power of God to change homosexual practice. Health care reform needs to be accomplished not just because of the economics but also because there are injustices in the current system. The church has always been involved in healing; it needs to renew that responsibility in creative new ways. Finally the AIDS epidemic should cause our society to question moral relativism. Prevention of AIDS for us and our children will require us to try to change our society by changing the public media and banning pornography. Medical ethics teaches us that the Gospel is inherently social. As Christians in the world of science, we must integrate scientific knowledge and Biblical truth; from this base we must help the church move to appropriate social action.
References
Annas, G.J. and Elias S: "The Politics of Transplantation of Human Fetal Tissue." N Engl J Med 320 (1989): 1079.
Bailey, J.M. and Pillard, R.C.: "A Genetic Study of Male Sexual Orientation." Arch Gen Psychiatry 48 (1991): 1089-95.
Bone, R.C., Rackow, E.C. and Weg, J.G., et. al.: "Ethical and Moral Guidelines For the Initiation, Continuation, and Withdrawal of Intensive Care." Chest 97 (1990): 949-958.
Briere, J.: "Medical Symptoms, Health Risk and History of Childhood Sexual Abuse." May Clin Prac 67 (1992): 603-604.
Brundin, P., Bjorklund, A. and Lindvall, O.: "Practical Aspects of the Use of Human Fetal Brain Tissue For Intracerebral Grafting" in Dennett, S.B and Richards, S.J., Eds. Progress in Brain Research, Elsevier Science. New York, NY 82 (1990): 707-714.
Burton, T.M.: "Firms That Promise Lower Medical Bills May Increase Them." Wall Street J 27 July 92, p. A1, A6.
Colson, C. and Vaughn, E.S.: The Body: Being Light in Darkness. Word Publishing Dallas 1992, pp. 297-8.
Consultants to the Advisory Committee to the Director of National Institutes of Health. Report of the Human Fetal Tissue Transplantation Research Panel Vol I. National Institutes of Health Bethesda, MD 1988.
Duggins, D.: "The Euthanasia Battle." Moody Monthly. 92(8):60.
Fisher, J.C.: "The Silicone Controversy: When Will Science Prevail?" N Engl J Med 326 (1992): 1696-1698.
Freed, C.R., et al.: "Transplantation of Fetal Substantia Nigra and Adrenal Medulla to the Caudate Nucleus in Two Patients with Parkinson's Disease." N Engl J Med 319 (1988): 370.
Freed, C.R., et al. "Survival of Implanted Fetal Dopamine Cells and Neurologic Improvement 12 to 46 Months after Transplantation for Parkinson's Disease." N Engl J Med 327 (1992 ): 1549-1555.
Garry, D.J. et al. "Are There Really Alternatives to the Use of Fetal Tissue from Elective Abortions in Transplantation Research?" N Engl J Med 327 (1992): 1592-95.
Gilman, S.: "Advances in Neurology." N Engl J Med 326 (1992): 1608-1616.
Global AIDS News, WHO GPA, 1992 #1.
Hendricks, S.E., Graber, B., and Rodriguez-Sierra, J.F.: "Neuroendocrine Responses to Exogenous Estrogens: No Difference Between Heterosexual and Homosexual Men."<R>Psychoneuroendocrinology 14 (1989): 177-185.
Horgan, J.: "Death With Dignity." Scientific American 1991(3):17.
Hyman, C., Hofer, M., and Barda, Y.A., et. al.: ABDNF Is A Neurotrophic Factor For Dopaminergic Neurons of the Substantia Nigra." Nature 350 (1991): 230-232.
Johnson, Paul: Modern Times: The World from the Twenties to the Eighties. Harper and Row New York 1983.
Jones, D.: "Halifax Hospital First in Canada to Proceed with Controversial Fetal-tissue Transplant." Can Med Assoc J 146 (1992): 389-391.
LeVay, S.: "A Difference in Hypothalamic Structure Between Heterosexual and Homosexual Men." Science 253 (1991): 1034-1037.
Lipsitz, L.A. and Goldberger, A.L.: "Loss of 'Complexity` and Aging." J Am Med Ass 267 (1992): 1806-1809.
Minnery, T., Ed: Pornography: A Human Tragedy. Tyndale House Wheaton, Illinois 1986, pp 115-186.
Morbidity and Mortality Weekly Report. 41 (1992): 945-950.
Multi-Society Task Force on PVS: Medical Aspects of the Persistent Vegetative State. N Engl J Med 330 (1994):1499-508,1572-1579.
Otto, D. and Unsicker, K.: "Basic FGF Reverses Chemical and Morphological Deficits in the Nigrostriatal System of MPTP-treated Mice." J Neurosci 10 (1990): 1912-1921.
Pankratz, R.C.: "Death Debate." CMDS Journal 13 (1992): (2): 12-15.
Parkinson Study Group. "Effect of Deprenyl on the Progression of Disability in Early Parkinson's Disease." N Engl J Med 321 (1989): 1364-1371.
Pattison, E.M. and Pattison, M.L.: "'Ex-gays`: Religiously Mediated Change in Homosexuals." Am J Psychiatry 137 (1989): 12.
Pellegrino, E.D. and Sharpe, V.A.: "Medical Ethics in the Courtroom: the Need For Scrutiny." Perspectives in Biology and Medicine 32 (1989): 547-564.
Post, S.G.: "Fetal Tissue Transplant: The Right to Question Progress." America 12 January 91, pp 14-16.
Quinn, Niall P.: "The Clinical Application of Cell Grafting Techniques in Patients With Parkinson's Disease" in Dunnett, S.B. and Richards, S.J. Progress in Brain Research, Elsevier Science New York, NY 1990, pp. 619-625.
Schiedermayer, D.: "The Death Debate." CMDS Journal 12 (1991): 13-19.
Skoog, T. et al.: "A Population-based Study of Dementia in 85-year-olds." N Engl J Med 328 (1993): 153-158.
Sladek, J.R. and Shoulson, I.: "Neural Transplantation: A Call For Patience Rather Than Patients." Science 240 (1988): 1386-1389.
Spencer, D.D., et al.: "Unilateral Transplantation of Human Fetal Mesencephalic Tissue Into Caudate Nucleus of Patients with Parkinson's Disease." N Engl J Med 327 (1992): 1541-8.
Spudis, E.V.: "The Persistent Vegetative State: 1990." Neurol Sciences 102 (1991): 128-136.
Strong, Carson: "Fetal Tissue Transplantation: Can It Be Morally Insulated from Abortion?" J Med Ethics 17 (1991): 70-76.
The Child Neurology Society Ethics Committee: "The Persistent Vegetative State in Children: Results of the Questionnaire Sent to the Members of the Child Neurology Society." Ann Neurology 30 (1991): 472A.
Van der Maas, P.J., Van Delden, J.J.M., Pijnenborg, L., and Looman, C.W.N.: "Euthanasia and Other Medical Decisions Concerning the End of Life." Lancet 338 (1991): 669-74.
Wachter, R.M.: "AIDS, Activism and the Politics of Health." N Engl J Med 326 (1992): 128-133.
Weissman, G.: The Doctor Dilemma. Whittle Direct Books Knoxville, Tennessee 1992.
Whitcomb, M.E. and Desgroseilliers, J.P.: "Primary Care in Canada." N Engl J Med 326 (1992): 1469-1472.
Widner, H., et al.: "Bilateral Fetal Mesencephalic Grafting in Two Patients With Parkinsonism Induced by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)." N Engl J Med 327 (1992): 1556-63.
Witkin, G., Friedman, D., and Guttman, M.: "Health Care Fraud." U.S. News and World Report, 24 February 92, p 34.